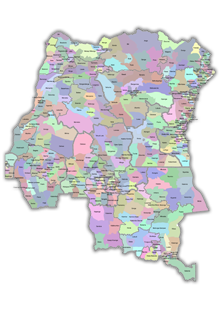
Mechanisms Used to Deliver Family Planning Services in the DRC
The Ministry of Health is the main State institution in charge with providing health services, including FP. Out of the 401 hospitals that exist in DRC, 176 belong to the government (compared to 179 to faith-based organizations (FBO) and 46 to public and private companies).
- Central Level:
- The Ministry of Health, the General Secretariat (secretariat general), 12 Divisions (known as “directions”), and 52 national programs , of which the National Program of Reproductive Health (PNSR) is one. PNSR was established to play a leadership role in coordinating family planning (and safe motherhood) services throughout the country.
- Intermediate Level:
- Provincial health inspection (inspection provincial de la santé), health zones (districts sanitaires)
- Operational level:
- Zones de santé (515 in total, of which 35 are in Kinshasa), with a reference hospital (hôpital général de référence) and health centers that deliver integrated health services to the population of the health zone.
In 2006, the Ministry of Health, in partnership with donors, developed a new strategy for health care delivery entitled the Stratégie de Renforcement du Système de Santé (SRSS), which defined the health zones as the entry point for all health interventions. The goal was to improve the supply of health services and quality of health care for the entire population of the DRC. The health zone approach was an effective method for health care delivery when implemented in the 1980s before the civil conflict.
All health care services are now delivered at the health zone level and the government has established guidelines for a Minimum Package of Activities (MPA) including basic curative care, immunization, reproductive health and child spacing, maternal care, malaria, TB, HIV/AIDS and blood safety, and drug supply.
Both reference hospitals and health centers are expected to deliver family planning as part of the Minimum Package of Activities. According to the MOH, DRC currently has 401 hospitals, 8,126 health centers and an unknown number of other health facilities. However, due to the chronic shortage of human, material, and financial resources, a great majority of existing facilities do not offer all, or even most, of the services they are expected to provide, including those within the minimum package. The actual delivery of family planning services, including availability of contraceptives, varies greatly by facility and depends on several key factors:
- Is the health facility supported by a donor (USAID, UNFPA, World Bank, DfID, CIDA, or other)? During the life of such projects, facilities are likely to have resources to provide a range of health services, including FP. However, at present, over 200 of the 515 DRC health zones do not receive donor support for health.
- Is the support ”global” (comprehensive) or disease-specific? Global/comprehensive assistance generally supports the delivery of an integrated package of services (the MPA), including family planning. In contrast, disease-specific funding (e.g., HIV, malaria) does not.
- Is the health facility operated by the Catholic Church? Management by the Catholic Church is likely to result in the non-delivery of modern or “artificial” contraception.
- Is the health facility operated by a private company (such as a mining company)? Companies are likely to have the resources to provide a range of health services, including FP.
PRIVATE, NON-PROFIT SECTOR, INCLUDING NGOs
This sector is no longer limited to the churches, although FBOs remain the major and often most stable player in the social sector. Numerous secular organizations, both local and international, have joined the FBOs. In the health sector, several PVOs (private voluntary organizations) provide family planning services in the DRC (see “FP organizations”). FP services are provided through one of the following mechanisms: (1) clinic-based integrated services; (2) social marketing; (3) community outreach; (4) provision by a stand-alone clinic.


1. Clinic-Based Integrated Health Services
This delivery model entails the delivery of FP services
through existing facilities in the health zones as an
integral part of the MPA. However, chronic shortages of
financial, material and human resources make it difficult
for a large proportion of health centers and health posts
to offer all, or even most, of the services included in
the MPA. Hence, the actual delivery of family planning
services, including availability of contraceptives,
varies greatly. In spite of this constraint, many donors
in DRC work through this model. Examples include the following:
- CIDA: will soon start a new program in 7 health zones in Kinshasa
- DfID: is increasing the number of zones from 20 to over 30 that will deliver FP as part of an integrated health services
- UNFPA: supports integrated health in 20 health zones of 4 provinces
- USAID: provides technical support and commodities to
health zones through its partner agencies, including:
- World Bank, which has financed the delivery of integrated health services in 80 zones, including FP, but is currently awaiting the lifting of a temporary blockage of funds invested in the DRC
2. Social Marketing
This delivery model is relatively underdeveloped in the
DRC, in contrast to many developing countries with highly
visible marketing campaigns for condoms and other
socially-marketed products. Only two organizations have
social marketing programs in the DRC, namely: PSI and DKT-RD Congo.
PSI’s social marketing program has consisted primarily of
ensuring a steady supply of products to health centers and
pharmacies through its Confiance and
Advancing Social Marketing for Health in the Democratic Republic of Congo
projects. PSI, which has operated continuously in the DRC
since 2003, uses point of sales advertising with a limited
amount of mass media marketing. DKT-RD Congo began its
activities in DRC in July 2010. It promotes DKT-RD Congo
branded condoms (OK Condoms), oral contraceptive pills,
and IUD. It will begin selling all products under its own
brand in 2012 via its social marketing program. At present,
DKT-RD Congo is operating in Kinshasa, Bas Congo, Katanga, and Bandundu
through its sales people at private sector outlets, including
wholesalers, pharmacies, clinics, and non-traditional outlets.
Training of clinic based providers and pharmacists and
community mobilizers is also being conducted. DKT will be
expanding to other provinces in 2013 and will be adding
additional family planning products to its portfolio.
3. Community-Based Distribution or Outreach
Community-based distributors (CBD) do not have formal
clinical training, but undergo short-term training provided
by that programs that enables them to deliver basic care for
specific conditions included in the MPA. As such, FP is one
of 10-12 areas that may fall within their job description.
Typically, CBDs offer a limited range of methods, often
just pills, condoms, CycleBeads®, and (only rarely)
injectable. This model of service delivery, relatively
uncommon in the DRC, is usually set up by PVOs. ABEF, the
IPPF member association in DRC, is one of the organizations
that rely on this mechanism of delivery. It reports having
155 CBD workers in Kinshasa alone. A second example is the
IRH, which assisted the Muslim organization – Maman Ansar –
to establish a CBD program in Kinshasa in 2011, with an
estimated 66 volunteers participating in the program (including
14 Imams, 40 CBDs, and 12 clinical providers). The WWF offers
services in Salonga National Park using a network of CBD workers.
4. Stand-Alone Clinic
Described as “vertical programs,” stand-alone clinics
provide family planning as their sole or primary service.
In some cases, these facilities provide other reproductive
health services (such as pap smears or HIV testing) but not
the MPA. FP stand-alone clinics are rare in DRC. The capital
city of Kinshasa has only three outlets that use this approach,
namely the Kintambo PNSR center, named Libota Lilamu and
two clinics operated by ABEF (although these two clinics provide
other maternal and child health services). This type of service
delivery focused largely on family planning is the rare
exception to the general rule of integration of FP into
a broader range of services.
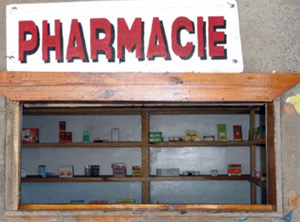
COMMERCIAL PRIVATE SECTOR
 The commercial sector includes private for-profit businesses owned by single
owners, partners, or corporations. Among its elements are also the
state-owned companies, such as the Société Nationale
d’Electricité (SNEL), the Société Nationale
de Chemins de Fer du Congo (SNCC), the
Générale des Carrières des Mines
(GECAMINES), the Minière de Bakwanga (MIBA),
and the Office National de Transport (ONATRA).
Prior to their recent collapses, some of the state-owned
companies were important sources of health services, not
only for their workers and their workers’ families but also
for the general population, particularly in the Maniema,
Katanga, and Kasai provinces. The commercial private sector
is often the
only meaningful source of supply for health facilities
located in health zones that have little to no support
from local NGOs or international donors. The private
for-profit pharmaceutical sector owns a large number of
pharmacies, mainly in large urban areas, particularly in
Kinshasa. Contraceptives, especially condoms, are available
at many pharmacies.
The commercial sector includes private for-profit businesses owned by single
owners, partners, or corporations. Among its elements are also the
state-owned companies, such as the Société Nationale
d’Electricité (SNEL), the Société Nationale
de Chemins de Fer du Congo (SNCC), the
Générale des Carrières des Mines
(GECAMINES), the Minière de Bakwanga (MIBA),
and the Office National de Transport (ONATRA).
Prior to their recent collapses, some of the state-owned
companies were important sources of health services, not
only for their workers and their workers’ families but also
for the general population, particularly in the Maniema,
Katanga, and Kasai provinces. The commercial private sector
is often the
only meaningful source of supply for health facilities
located in health zones that have little to no support
from local NGOs or international donors. The private
for-profit pharmaceutical sector owns a large number of
pharmacies, mainly in large urban areas, particularly in
Kinshasa. Contraceptives, especially condoms, are available
at many pharmacies.
A survey by the Kinshasa School of Public Health in 2012 identified over 1,600 pharmacies in Kinshasa that sold at least one type of contraceptive. Of the total number, the percent selling different methods was as indicated below. The table below indicates distribution of sources of supply for the 5.8% of married women of reproductive age that reported using a modern contraceptive method on the latest DHS study (2007).
PERCENT OF PHARMACIES AND HEALTH FACILITIES IN KINSHASA THAT SELL THE FOLLOWING CONTRACEPTIVE METHODS
| Method | Pharmacies (n=1646) | Pharmacies (n=1646) | Health Facilities (n=226) | Health Facilities (n=226) |
|---|---|---|---|---|
| % that usually have FP products in stock | % that had FP products in stock the day of the survey | % that usually have FP products in stock | % that had FP products in stock the day of the survey | |
| Pills | 38.2% | 32.3% | 53.5% | 51.3% |
| Condoms | 64.0% | 62.0% | 59.7% | 56.2% |
| IUD | 0.9% | 0.7% | 38.5% | 35.4% |
| Implants | 0.5% | 0.2% | 21.2% | 17.7% |
| Injectables | 33.8% | 27.8% | 64.2% | 61.1% |
| Spermicides | 0.8% | 0.7% | 2.7% | 1.8% |
SHORTCOMINGS IN SERVICE DELIVERY FOR FAMILY PLANNING AND REPRODUCTIVE HEALTH
Ideally, service delivery entails multiple activities: counseling the client regarding different contraceptive options, conducting a physical exam or administering a checklist to rule out complications (for certain methods), providing the client with a method (ideally, her preferred method, unless medically inadvisable), and giving information on follow-up and what to do in case of problems.
In its Annual Report for 2010, the PNSR lists the following shortcomings in service delivery (page 13) : PNSR Anuual Report
- Low coverage of RH services
- Low quality of RH services
- Poor integration of RH services in the health zones
- Lack of structural support
- Inadequate and obsolete infrastructure and equipment
| Source | Percent
Married Women | Percent
Married Women | Percent
All Married Women |
|---|---|---|---|
| in Kinshasa | outside Kinshasa | 15-49 | |
| Public Sector | 18.7 | 34.1 | 29.8 |
| Hospital | 8.7 | 23.1 | 19.1 |
| Clinic | 2.2 | 0.0 | 0.6 |
| Health Center | 6.9 | 9.8 | 9.0 |
| Maternity Center | 0.9 | 1.2 | 1.1 |
| Private Sector | 72.5 | 53.2 | 58.5 |
| Hospital/Private Clinic | 6.9 | 6.6 | 6.7 |
| Pharmacy | 54.8 | 38.8 | 43.2 |
| Amo-Congo | 2.3 | 0.1 | 0.7 |
| Health Center | 5.0 | 5.4 | 5.3 |
| Private Doctor | 0.0 | 0.1 | 0.05 |
| Ambulatory Nurse | 0.0 | 0.5 | 0.3 |
| Health Worker | 0.0 | 1.1 | 0.9 |
| Other | 3.5 | 0.5 | 1.3 |
| Other Source | 8.9 | 12.3 | 11.4 |
| Shop | 2.8 | 1.4 | 1.8 |
| Church | 0.9 | 0.0 | 0.3 |
| Parents/Friends | 5.2 | 10.9 | 9.3 |
| Total (100%) | n=102 | n=268 | n=370 |